Accessible ways to prevent cervical cancer in Japanese women
Research Highlight | March 30, 2020
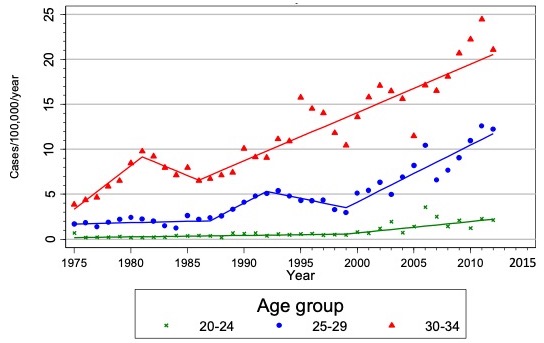
According to the National Cancer Center Japan, cervical cancer is increasing in Japanese women of reproductive age. Cervical cancer is a cancer that occurs at the neck of the uterus, the cervix, and is caused by the human papillomavirus (HPV). There are 12–15 high-risk types of HPV that cause cervical cancer and HPV are usually sexually transmitted. Types 16 and 18 in particular cause around 70% of cervical cancer globally. HPV 16 is also responsible for most all other HPV-related cancers such as anal cancer and vaginal cancer.
Unlike most cancers, cervical cancer is preventable. There are 2 approaches to the prevention. The first is through vaccination, and second is through regular screening which can detect HPV infection or abnormal cells before they become cancerous. “Combining both approaches is clearly the most effective way to prevent cervical cancer,” says Dr. Sharon Hanley, a cancer epidemiologist at Hokkaido University.
While most HPV infections clear within 2 years, 10% may persist. Having a persistent infection increases the risk of developing a precancer or ultimately an invasive cancer. “Fortunately, an HPV 16 and HPV 18 infection can be prevented with a safe and effective vaccine,” says Dr. Hanley. “The vaccine is free for all Japanese girls aged 12-16yrs and I would strongly recommend that parents use this opportunity to have their daughters vaccinated.”
If a high-grade precancer develops it needs to be removed via a small surgical procedure before progression into invasive cervical cancer. “The process from infection to invasive cancer takes many years and that is why regular cervical screening is so important,” Dr. Hanley explains.
Dr. Hanley and her team are looking to establish easier and more accessible ways to increase the rate of screening for cervical cancer in young women in Japan.
The National Cancer Center Japan recommends regular screening once every two years, but coverage is low at 30-40%. “Lack of awareness about cervical cancer, stigma associated with visiting a gynecologist, fear of the test and embarrassment are reasons why Japanese women don’t go for screening,” says Dr. Hanley. “Sadly, many Japanese women go to the gynecologist for the first time when they are pregnant and this overlaps with the age at which high-grade precancers and invasive cervical cancer are most common. So, finding out you are pregnant and also having cervical cancer is not so rare here.”
To help empower women to undergo cervical screening, Dr. Hanley and the Department of Reproductive and Developmental Medicine at the Graduate School of Medicine, in collaboration with Hokkaido Cancer Society, have been piloting HPV self-sampling, a method where women take a vaginal sample using a device sent to them through the post, to test if the sample is positive for HPV-DNA. Compared to a pap smear, HPV self-sampling is non-invasive and more accessible for all women, in particular for young women who may be working full-time or have young children to look after, since women don’t need to go to a gynecologist.
Dr. Hanley’s group asked women to undergo self-sampling when they had their annual workplace health check-up. The women also underwent screening by a doctor. They found that women reported self-sampling to be significantly less embarrassing, less painful, and less stressful than the doctor’s test. “Importantly, our study showed self-sampling is as effective and accurate in picking up HPV infections as the doctors test, as with other studies worldwide,” says Dr. Hanley. “Over 90% of women who underwent self-sampling said they would recommend it to their friends and family.”
The next step for Dr. Hanley’s team is to look at women’s preferences for self-sampling devices since the researchers regard it as very important to make the device mentally accessible for Japanese women. They are now analyzing the users’ impressions of 3 types of devices to clarify preferences in shape, texture, ease of use and also color.
“HPV self-sampling is a highly sensitive and highly acceptable method of cervical screening that can also be used to address the shortage of gynecologists in rural Hokkaido,” says Dr. Hanley. The team has plans to promote HPV self-sampling with more regional governments in Hokkaido to adopt it in their screening program. “No woman in Japan should have to endure the unnecessary pain and suffering from cervical cancer. We hope our research will help empower women to take active measures against the disease.”
Written by Yuki Otani (Science Writing Intern)