New therapy target for malignant melanomas in dogs
Research Press Release | April 22, 2021
Scientists have shown that the biological molecule PD-L1 is a potential target for the treatment of metastasized oral malignant melanoma in dogs.
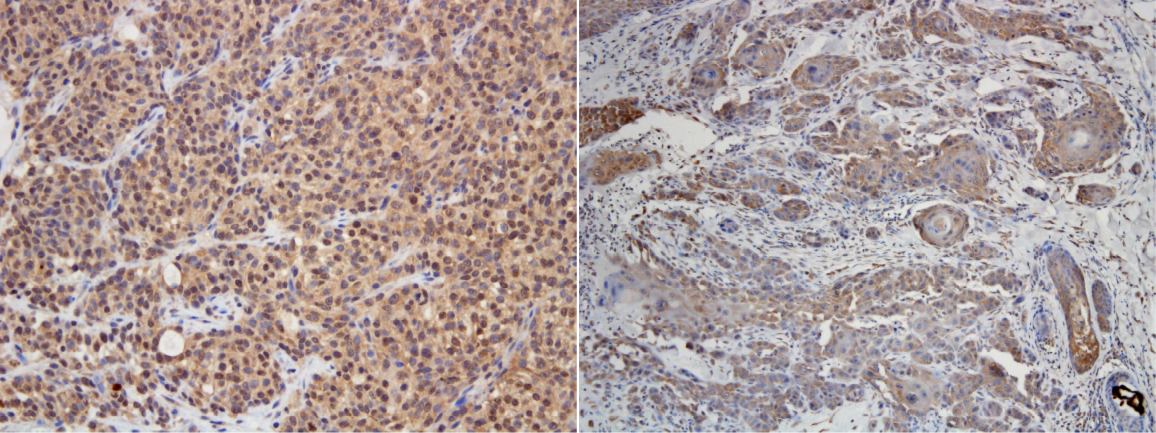
PD-L1 immunohistochemical staining in typical oral malignant melanoma (left) and squamous cell skin cancer (right). The tumor cells are stained brown, indicating that they are PD-L1 positive (Naoya Maekawa, et al. npj Precision Oncology. February 12, 2021).
There are a number of cancers that affect dogs, but there are far fewer diagnosis and treatment options for these canine cancers. However, as dogs and humans are both mammals, it is likely that strategies and treatments for cancers in humans can be used for canine cancer, with minor modifications.
A team of scientists, including Associate Professor Satoru Konnai from the Faculty of Veterinary Medicine at Hokkaido University, have demonstrated that an anti-cancer therapy that targets the cancer marker PD-L1—a target that has shown great promise for treating cancer in humans—is effective for canine cancer as well. Their findings were published in the journal npj Precision Oncology.
The proteins Programmed Cell Death 1 (PD-1) and its associated molecule, PD-ligand 1 (PD-L1) are involved in the immune response in humans. PD-L1 is overexpressed by many types of cancer in humans, enabling these cancers to suppress the immune response. Studies in mice models and in human cell lines have shown that PD-1 and PD-L1 have great promise in the treatment of cancer as blocking them strengthens the immune response to cancer.
Malignant melanomas are a canine cancer that is both relatively common and fatal. In particular, oral malignant melanomas (OMMs) are highly invasive and metastatic; with treatment, the median survival time is less than two months. As new treatments are needed for this cancer, the scientists chose to explore the options available.
The scientists first developed a novel anti-PD-L1 monoclonal antibody to detect PD-L1 in various canine cancers by immunohistochemical staining. Using this antibody, they demonstrated that malignant canine cancers expressed PD-L1; out of 20 samples for each cancer tested, nasal adenocarcinoma, transitional cell carcinoma, osteosarcoma and mammary adenocarcinoma had a 100% positive rate, while anal sac gland carcinoma and OMM had a 95% positive rate.
A prior pilot study had shown that another canine chimeric anti-PD-L1 monoclonal antibody had anti-tumor effect against OMM, when tested on nine dogs. For the current study scientists selected 29 dogs with primary OMM and pulmonary metastasis, where the melanoma has spread to the lungs, and most of which had been subjected to at least one round of treatment. These dogs were treated with the chimeric antibody every two weeks, and other interventions to achieve local control of cancer were allowed.
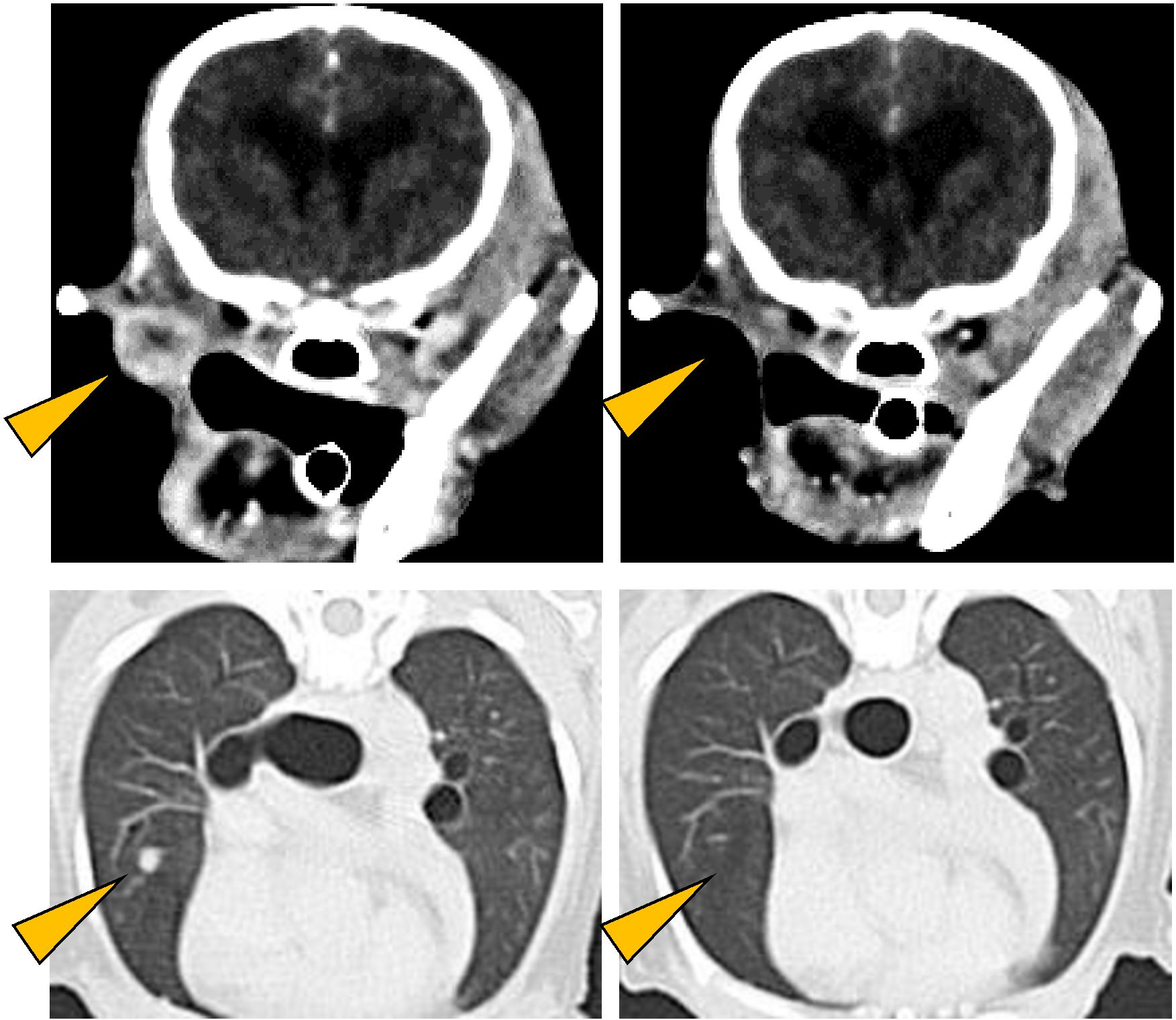
Antitumor effect of anti-PD-L1 antibody. CT images of oral malignant melanoma (upper left) and its lung metastases (lower left) observed in a Pomeranian (12 years old, male). As a result of treatment with anti-PD-L1 antibody, all detectable tumors disappeared (right panels; Naoya Maekawa, et al. npj Precision Oncology. February 12, 2021).
The survival time of dogs treated with the chimeric antibody was significantly longer, with a median survival time of 143 days, compared to 54 days for the control group, from historical data. Thirteen dogs had measurable cancer (i.e., at least one tumor >10 mm in diameter in CT scan), while 16 had non-measurable cancer (all tumors < 10 mm in diameter in CT scan). Five dogs showed tumor response, where the tumor reduced or disappeared due to the treatment. In one of these, all detectable tumors disappeared. In two other dogs, all detectable tumors disappeared, resulting in survival times longer than a year. In the last two dogs, all tumors in the lungs disappeared, but oral and lymph node tumors persisted. The increase in survival time correlated positively with radiation therapy that was simultaneous or began within eight weeks of treatment with the chimeric antibody.
“Our findings are limited by the small size of the historical control group,” says Satoru Konnai. “Nevertheless, as there is no systemic therapy that prolongs the survival of dogs with pulmonary metastatic OMM, the increased survival time encourages the further development of anti-PD-L1 therapy in dogs.”

From the left: Yusuke Izumi, Naoya Maekawa, Satoshi Takagi, Tatsuya Deguchi and Satoru Konnai, members of the research team (Photo: Hokkadio University).
Original Article:
Naoya Maekawa, et al. PD-L1 immunohistochemistry for canine cancers and clinical benefit of anti-PD-L1 antibody in dogs with pulmonary metastatic oral malignant melanoma. npj Precision Oncology. February 12, 2021.
DOI: 10.1038/s41698-021-00147-6
Funding:
This work was supported by the Grant-in-Aid for Scientific Research (16K15042, 19H03114, and 19K15969) and Grant-in-aid for JSPS Fellows (15J01989) from the Japan Society for the Promotion of Science (JSPS) and by Japan Agency for Medical Research and Development (AMED; JP20am0101078).
Contacts:
Associate Professor Satoru Konnai
Laboratory of Infectious Diseases
Faculty of Veterinary Medicine
Hokkaido University
Tel: +81-11-706-5216
Email: konnai[at]vetmed.hokudai.ac.jp
Sohail Keegan Pinto (International Public Relations Specialist)
Public Relations Division
Hokkaido University
Tel: +81-11-706-2185
Skype: hokudai.pr1
Email: en-press[at]general.hokudai.ac.jp
Related Articles:
Developing immunotherapy to save animals
New therapeutic antibody for dog cancers
